Health Care Showdown: Kennedy's Vision Clashes with Trump's Budget Ax
Health
2025-02-14 11:06:49Content
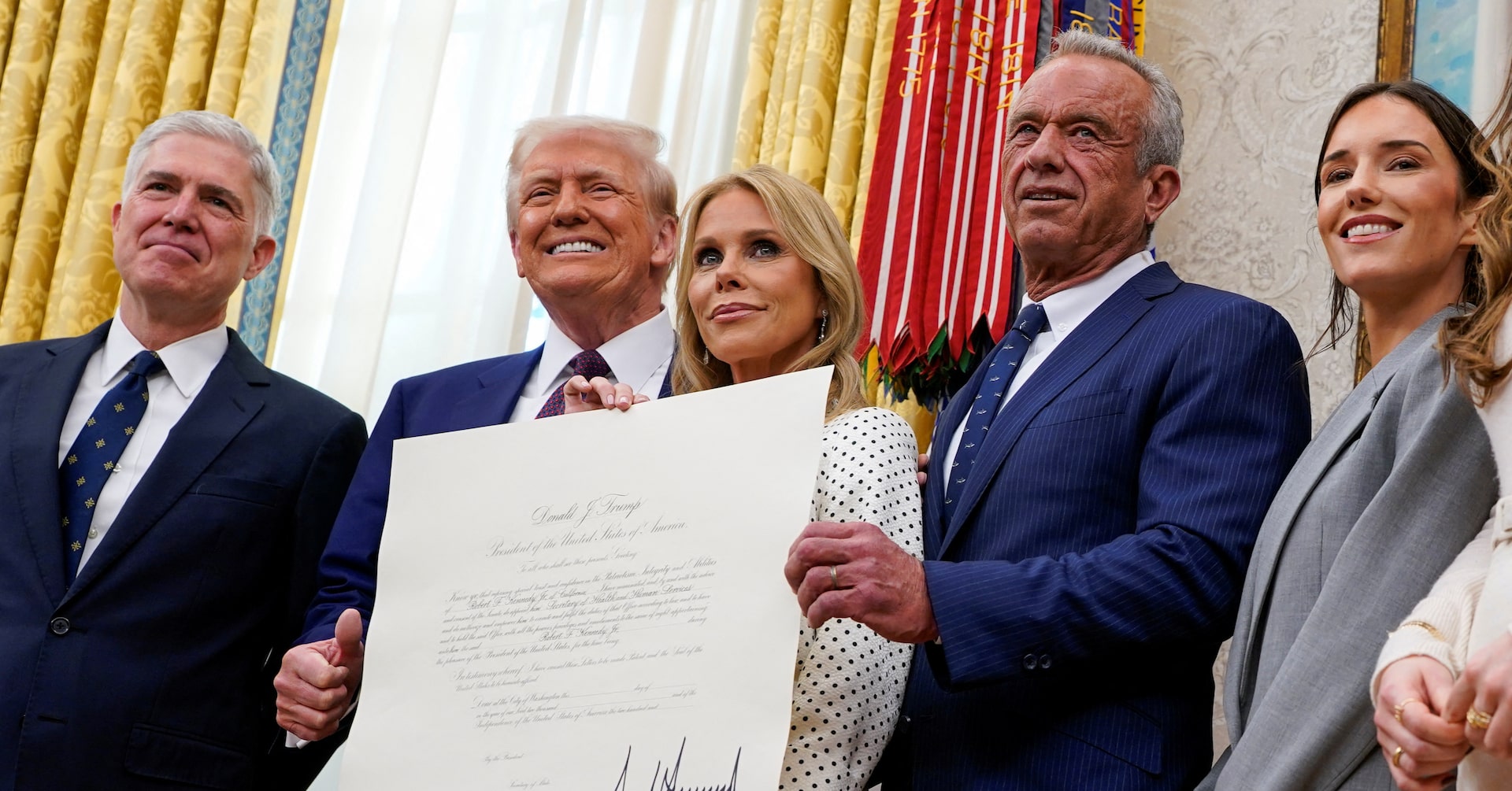
Robert F. Kennedy Jr. Embarks on Ambitious Health Mission with Presidential Support
In a bold move to tackle the growing challenge of chronic illness, Robert F. Kennedy Jr. has stepped forward with an ambitious health agenda, backed by President Donald Trump. The newly appointed U.S. health secretary is set to launch a comprehensive approach to improving national health, targeting everything from food quality to vaccine research.
However, Kennedy's wide-ranging plans may face significant hurdles as they potentially conflict with ongoing government spending reductions. His vision encompasses transformative strategies to address the nation's health challenges, including initiatives to enhance nutritional standards and conduct in-depth studies on vaccination protocols.
The proposed agenda signals a potentially groundbreaking approach to public health, promising to challenge existing healthcare paradigms while navigating the complex landscape of federal budgetary constraints. Kennedy's commitment to addressing chronic illness represents a potentially pivotal moment in U.S. healthcare policy, with implications that could reshape how the nation approaches medical prevention and treatment.
Health Revolution: Navigating the Complex Landscape of Public Health Policy and Innovation
In the ever-evolving realm of public health, leadership transitions bring both promise and potential challenges. The appointment of a new health secretary represents a critical moment of potential transformation, where innovative approaches and strategic vision can reshape the nation's healthcare trajectory.Pioneering Change: A Bold Vision for National Health Transformation
Reimagining Healthcare Infrastructure
The contemporary healthcare landscape demands a multifaceted approach that transcends traditional boundaries. Comprehensive health strategies require intricate understanding of systemic challenges, technological innovations, and emerging medical paradigms. Policymakers must navigate complex intersections between preventative medicine, technological intervention, and holistic wellness frameworks. Modern healthcare transformation necessitates radical rethinking of existing infrastructures. By integrating cutting-edge research, advanced diagnostic technologies, and patient-centered care models, we can develop more responsive and adaptive health systems. This approach demands collaborative efforts across multiple disciplines, including medical research, technology development, and public policy implementation.Nutritional Policy and Public Health Strategies
Nutritional interventions represent a critical frontier in public health management. Comprehensive food policy reforms can potentially mitigate numerous chronic health conditions by addressing fundamental dietary challenges. Implementing evidence-based nutritional guidelines requires sophisticated understanding of metabolic processes, cultural dietary practices, and socioeconomic factors influencing food consumption patterns. Emerging research suggests that targeted nutritional interventions can significantly impact population health outcomes. By developing nuanced strategies that consider individual metabolic variations, genetic predispositions, and environmental influences, policymakers can create more personalized and effective health promotion frameworks.Vaccine Research and Scientific Accountability
Vaccine development and research represent a complex and dynamic field of scientific inquiry. Rigorous scientific methodologies, transparent research protocols, and comprehensive safety evaluations are paramount in maintaining public trust and advancing medical knowledge. Balancing scientific innovation with robust safety mechanisms requires sophisticated regulatory frameworks and interdisciplinary collaboration. The ongoing evolution of vaccine technologies demands continuous adaptation and critical evaluation. By fostering environments that encourage open scientific dialogue, support independent research, and prioritize evidence-based decision-making, we can develop more effective and trustworthy medical interventions.Budgetary Constraints and Strategic Prioritization
Healthcare innovation exists within intricate financial ecosystems characterized by competing priorities and limited resources. Strategic budget allocation requires nuanced understanding of long-term public health objectives, potential return on investment, and comprehensive impact assessment methodologies. Navigating fiscal constraints demands creative problem-solving, leveraging technological efficiencies, and developing scalable intervention models. By implementing data-driven decision-making processes and exploring innovative funding mechanisms, policymakers can maximize healthcare investments while maintaining fiscal responsibility.Technological Integration and Future Healthcare Models
Digital technologies are fundamentally reshaping healthcare delivery paradigms. Artificial intelligence, machine learning, and advanced diagnostic tools offer unprecedented opportunities for personalized medical interventions, predictive healthcare strategies, and enhanced patient outcomes. The convergence of technological innovation and medical expertise creates exciting possibilities for transformative healthcare models. By embracing interdisciplinary approaches and fostering collaborative research environments, we can develop more responsive, efficient, and patient-centered healthcare systems.RELATED NEWS
Health

Nourishing Futures: Free Heart-Smart Pantry Serves Students Across North Texas
2025-02-28 21:58:58
Health

Holy Dedication: How Nuns Unlocked 3 Decades of Groundbreaking Dementia Research
2025-02-26 17:31:20
Health
AI Revolution: Chinese Health Tech Giants Embrace DeepSek's Cutting-Edge Technology
2025-02-24 11:09:46