Medicaid Oversight Breakdown: Louisiana's Health Department Drops the Ball, Audit Reveals
Health
2025-03-11 09:00:00Content

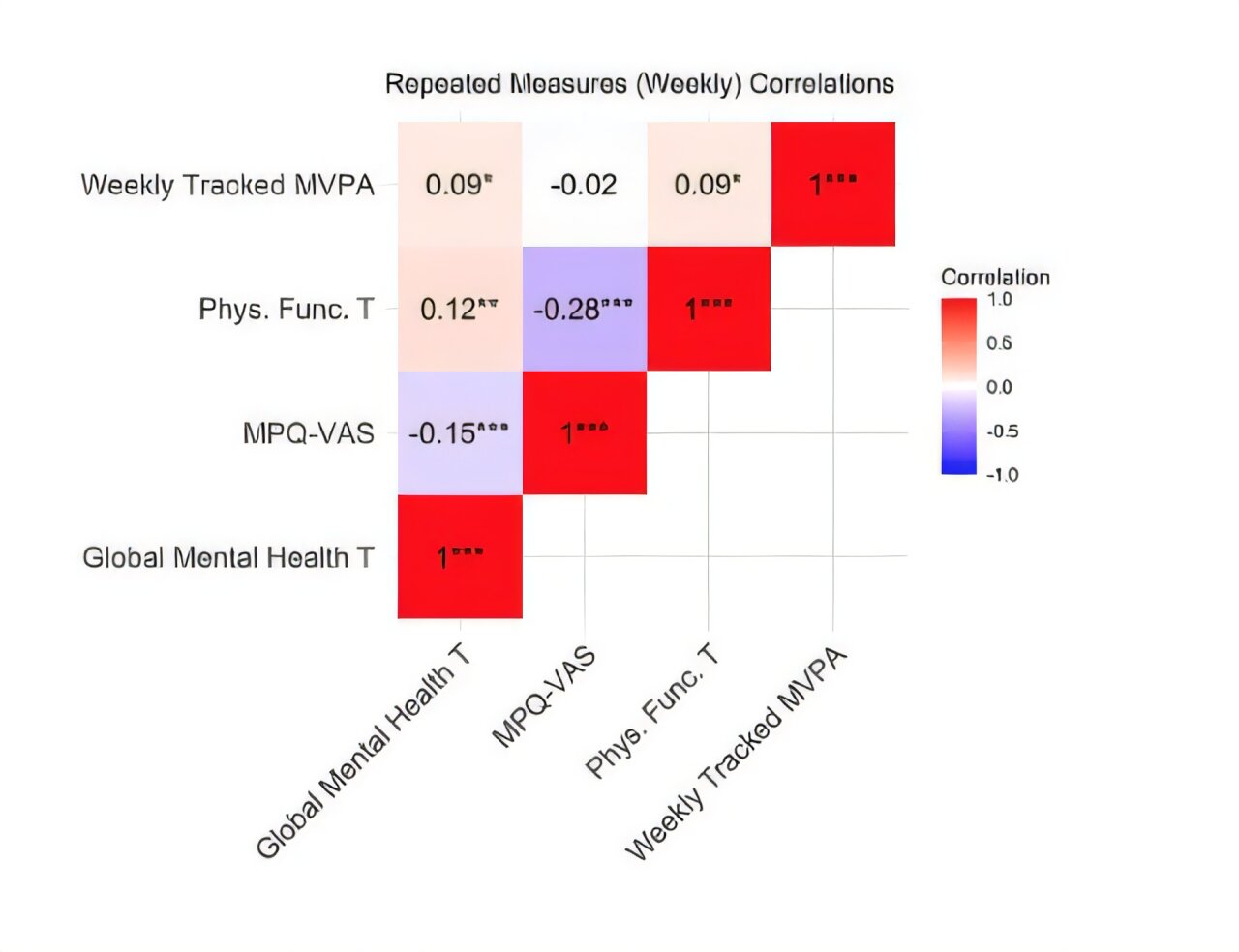
A recent audit has revealed significant inefficiencies in Louisiana's Medicaid incentive program, with over 50% of allocated funds being diverted to administrative overhead and activities that cannot be effectively measured for their impact on healthcare outcomes.
The findings raise serious questions about the program's effectiveness and transparency. Instead of directly improving health access for Louisiana residents, a substantial portion of the program's budget appears to be consumed by bureaucratic processes and non-essential expenditures.
This audit exposes potential systemic issues within the state's healthcare funding mechanism, suggesting an urgent need for comprehensive review and restructuring. Policymakers and healthcare administrators must now critically examine how these funds can be more strategically deployed to genuinely enhance medical services and patient care.
The revelation underscores the importance of rigorous financial oversight and the need to ensure that healthcare incentive programs truly deliver tangible benefits to the communities they are designed to serve.
Medicaid's Murky Millions: Louisiana's Healthcare Funding Facade Exposed
In the labyrinthine world of healthcare funding, a startling revelation has emerged from the heart of Louisiana, casting a long shadow over the state's Medicaid incentive program. The intricate dance of administrative spending and healthcare outcomes has once again brought to light the complex challenges facing public health infrastructure.Unraveling the Financial Maze of Healthcare Spending
The Administrative Overhead Conundrum
Louisiana's Medicaid program has become a microcosm of broader healthcare funding challenges, with an unprecedented proportion of resources seemingly evaporating into administrative black holes. Investigative analysis reveals a troubling pattern where more than half of allocated funds fail to directly impact patient care or health outcomes. This systemic inefficiency represents a critical juncture in healthcare resource allocation, challenging policymakers and healthcare administrators to reimagine funding strategies. The financial landscape exposes a stark disconnect between intended healthcare improvements and actual resource utilization. Experts argue that such administrative bloat not only undermines the program's core objectives but also represents a significant misallocation of taxpayer resources. The intricate web of bureaucratic processes appears to have created a self-perpetuating system that prioritizes internal mechanisms over direct patient care.Dissecting the Funding Mechanism
Deeper examination of the Medicaid incentive program unveils a complex ecosystem of financial distribution that raises significant questions about accountability and transparency. The audit's findings suggest a fundamental misalignment between program goals and actual resource deployment. Healthcare policy analysts point to systemic inefficiencies that have long plagued public health funding mechanisms. The financial forensics reveal a troubling narrative of bureaucratic complexity. Each dollar allocated becomes a journey through multiple administrative layers, with diminishing returns for actual healthcare delivery. This intricate dance of funding demonstrates the challenges inherent in large-scale public health initiatives, where good intentions often become entangled in bureaucratic red tape.Implications for Healthcare Access and Outcomes
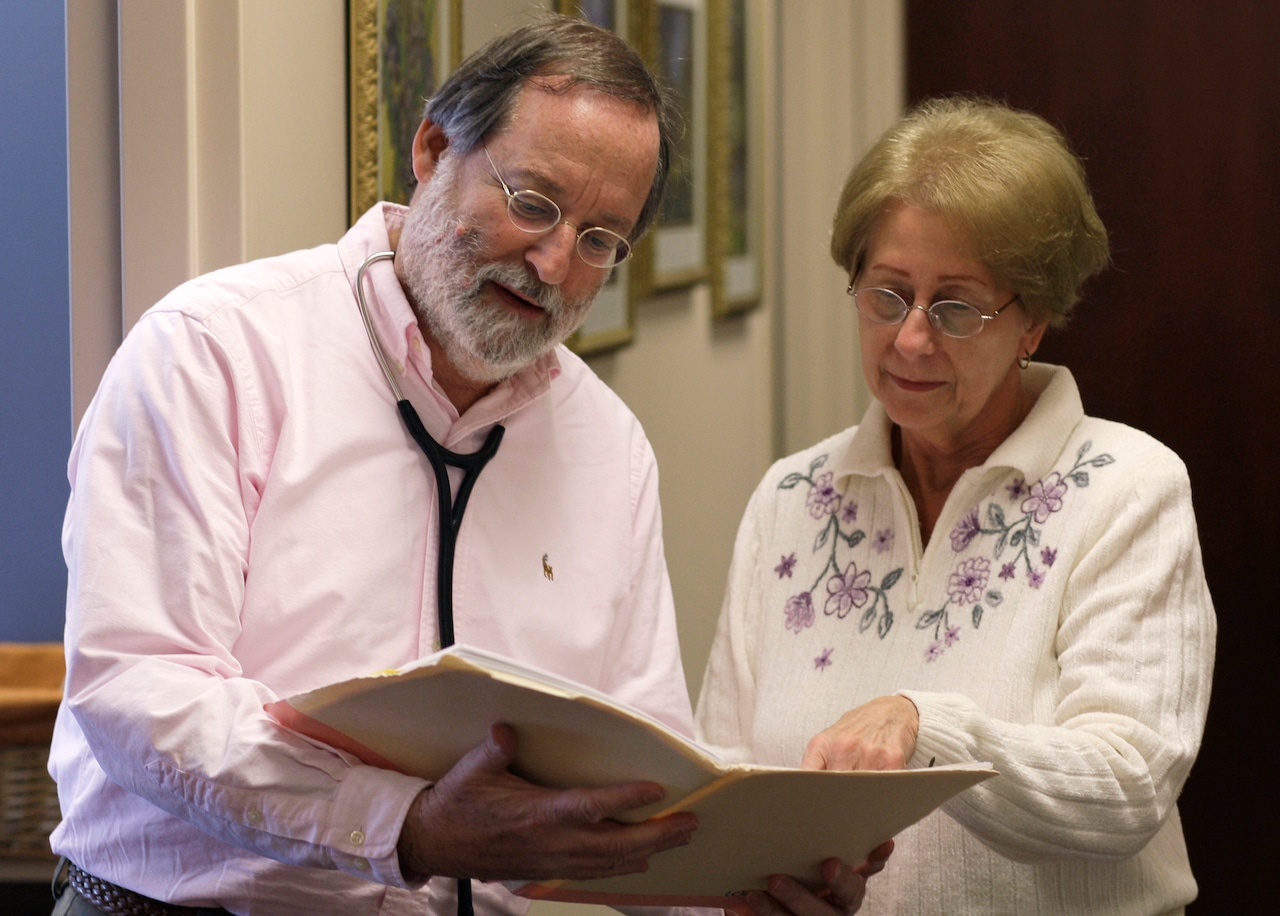
The ramifications of such administrative inefficiency extend far beyond mere financial concerns. Patients in Louisiana find themselves caught in a system where resources intended for direct healthcare support become trapped in a labyrinth of administrative processes. This systemic failure potentially compromises access to critical healthcare services for the most vulnerable populations. Healthcare advocates argue that every percentage point of administrative spending represents a direct opportunity cost for patient care. The audit serves as a critical wake-up call, demanding a comprehensive reevaluation of how public health funds are conceptualized, allocated, and ultimately utilized. It challenges the fundamental assumptions underlying current healthcare funding models.A Call for Transformative Accountability
The revelations demand more than mere criticism – they necessitate a fundamental reimagining of healthcare resource management. Policymakers, healthcare administrators, and community stakeholders must collaborate to develop more transparent, efficient funding mechanisms that prioritize patient outcomes over administrative complexity. Innovative approaches are needed to break the cycle of bureaucratic inefficiency. This might involve implementing more rigorous oversight, developing real-time tracking mechanisms, and creating incentive structures that directly reward measurable healthcare improvements. The path forward requires a delicate balance between administrative necessity and direct patient care support.RELATED NEWS
Health
Medicaid Cuts Threaten Healthcare for Nearly 800,000 Ohioans: GOP's Radical Overhaul Sparks Alarm
2025-02-19 13:00:00